For individuals managing diabetes, dental health plays a surprisingly crucial role in maintaining stable blood sugar levels. Emerging research reveals a bidirectional relationship between diabetes and oral health, where poor oral hygiene can exacerbate diabetes and vice versa. Understanding this connection can help individuals with diabetes develop effective strategies for blood sugar control and overall health.
The Connection Between Oral Health and Diabetes
Diabetes affects the body’s ability to regulate blood sugar, but it also has implications for oral health. High blood sugar levels increase the risk of gum disease, which, in turn, can make diabetes harder to control. Studies from the National Institute of Dental and Craniofacial Research indicate that diabetics are more prone to developing periodontal disease, an infection of the gums and bones that support the teeth. This risk makes it essential for diabetics to prioritize their oral hygiene as part of their diabetes management plan.
How Diabetes Increases the Risk of Gum Disease
People with diabetes are at a higher risk for gum disease due to a compromised immune system. When blood sugar levels are elevated, the body’s ability to fight infections weakens, allowing bacteria to thrive in the mouth. In a diabetic state, wounds heal more slowly, which means any gum inflammation or infection can persist and worsen. According to a study published in the Journal of Clinical Endocrinology & Metabolism, individuals with poorly controlled diabetes are up to three times more likely to develop severe gum disease than those without diabetes.
How Gum Disease Impacts Blood Sugar Levels
Gum disease doesn’t just remain in the mouth; it can lead to increased blood sugar levels, making diabetes more challenging to manage. When bacteria infect the gums, the immune system responds by releasing inflammatory markers. These markers can affect insulin sensitivity, leading to spikes in blood sugar. Addressing and preventing gum disease can help mitigate these blood sugar fluctuations, making diabetes management more stable and effective.
Dental Care Routines to Help Manage Blood Sugar Levels
A consistent and effective oral care routine can make a significant difference for diabetics. Maintaining oral health not only protects the teeth and gums but also supports overall health and blood sugar stability.
Regular Brushing and Flossing
Brushing at least twice a day with fluoride toothpaste and flossing daily are foundational habits for preventing gum disease. Brushing removes plaque from tooth surfaces, while flossing cleans between teeth and below the gumline, areas where plaque can quickly build up. For individuals with diabetes, these steps are particularly important because they help limit bacterial growth that could lead to inflammation and blood sugar spikes.
Using Antimicrobial Mouthwash
An antimicrobial mouthwash can reduce the bacteria that contribute to gum disease. Look for a mouthwash that is alcohol-free to avoid irritation. Using an antimicrobial mouthwash daily helps reduce bacterial load in the mouth, providing another layer of defense against gum inflammation and the associated impact on blood sugar.
Regular Dental Visits for Professional Cleanings
Routine dental visits are crucial for individuals with diabetes. Professional cleanings remove tartar buildup that cannot be eliminated with regular brushing and flossing alone. During these visits, a dentist can also monitor for early signs of gum disease and provide targeted treatments as necessary. For diabetic patients, visiting the dentist every six months is essential, though some individuals may need more frequent check-ups depending on their oral health status.
For more guidance on maintaining optimal dental health, especially for diabetics, Ames Dentistry offers comprehensive general dentistry services tailored to support overall health.
Lifestyle Adjustments to Support Oral and Blood Sugar Health
Beyond oral care, certain lifestyle choices can further support dental health and blood sugar control. Paying attention to diet and hydration, managing stress, and avoiding tobacco are all effective ways to protect both oral health and diabetes management.
Prioritizing a Balanced Diet
A balanced diet rich in nutrients strengthens both oral and systemic health. Foods high in vitamins A and C, such as leafy greens and citrus fruits, support gum health by boosting immunity. Fiber-rich foods can help stabilize blood sugar, preventing spikes and crashes. Avoiding sugary foods is particularly important for diabetics, as sugar contributes to both blood sugar increases and plaque buildup.
Staying Hydrated
Adequate hydration supports saliva production, which helps to wash away food particles and bacteria in the mouth. Diabetics often experience dry mouth due to certain medications or high blood sugar levels, which can lead to an increased risk of tooth decay and gum disease. Drinking water regularly can combat dry mouth and help reduce bacterial growth.
Managing Stress Levels
Chronic stress has a dual impact on both blood sugar and oral health. Stress can cause blood sugar levels to fluctuate, making diabetes harder to control, while also contributing to behaviors such as teeth grinding, which can damage teeth and gums. Practicing stress management techniques such as meditation, exercise, or spending time in nature can support both dental and diabetes management.
Avoiding Tobacco Products
Smoking and other forms of tobacco use can exacerbate both gum disease and diabetes complications. Tobacco reduces blood flow to the gums, slowing healing and weakening the immune response. Studies show that smokers with diabetes are at an even higher risk of developing periodontal disease. Quitting tobacco use can significantly improve both oral health and blood sugar control.
Recognizing Signs of Oral Health Issues for Diabetics
For diabetics, being vigilant about changes in oral health is important. Early recognition of symptoms like swollen gums, bleeding, or chronic bad breath can help prevent gum disease from worsening. If left untreated, these symptoms can escalate, leading to tooth loss and impacting blood sugar levels.
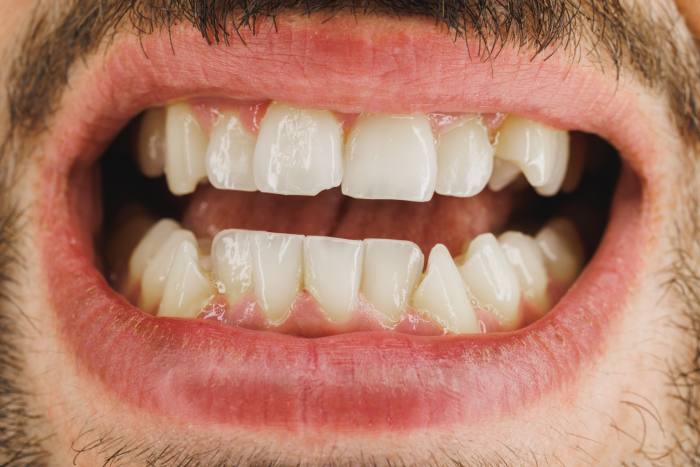
Common Symptoms of Gum Disease
Gum disease often begins with gingivitis, which presents as redness, swelling, and bleeding, particularly when brushing or flossing. Persistent bad breath, receding gums, and loose teeth are other indicators of gum disease. Diabetics who experience any of these symptoms should seek dental care promptly to prevent further complications.
Importance of Early Intervention
Treating gum disease early can prevent more severe conditions that may affect blood sugar control. Early intervention includes professional cleanings, scaling and root planing (deep cleaning), and targeted oral hygiene advice from your dentist. Research from the American Diabetes Association shows that managing periodontal health can lead to better glycemic control, making early intervention essential for diabetics.
Conclusion
For those managing diabetes, understanding the link between dental health and blood sugar levels is essential for comprehensive care. A consistent oral hygiene routine, regular dental visits, and a balanced lifestyle all contribute to maintaining both dental and diabetic health. Addressing gum disease proactively can support stable blood sugar levels, helping you manage diabetes more effectively.
To explore more about how dental care can support overall health, particularly for diabetic patients, Ames Dentistry provides a range of services aimed at promoting a healthy mouth and body. Additionally, the National Institute of Dental and Craniofacial Research offers valuable insights and information on the intersection of diabetes and dental health, helping you make informed decisions about your care.
By taking a proactive approach to dental health, individuals with diabetes can enjoy better control over their blood sugar, improved oral health, and a higher quality of life.